From admissions, to boarding, to transfers, to discharge – ensure a coordinated process
What if you could reduce the average patient stay by 4 hours, reduce ED boarding to less than 6 hours, or shave 35 minutes off the time it takes nurses to coordinate a transfer. These improvements not only help the profitability of Healthcare Delivery Organizations (HDOs), but they improve patient outcomes and can aid in staff retention. According to Gartner, “Cost and revenue pressures on healthcare delivery organizations continue to mount year over year. This underscores an abiding need for increased operational efficiency and continued digital innovation. HDO CIOs should leverage patient throughput and capacity management to satisfy both requirements.”[1]
There are many opportunities to streamline the flow of patients inside a hospital. A few of the major areas for improvement are
- Wait times in admissions
- Delays in handling transfers
- Wasted time locating equipment
- Delays in patient discharge
- Arranging and completing environmental services
Reducing Patient Wait Times
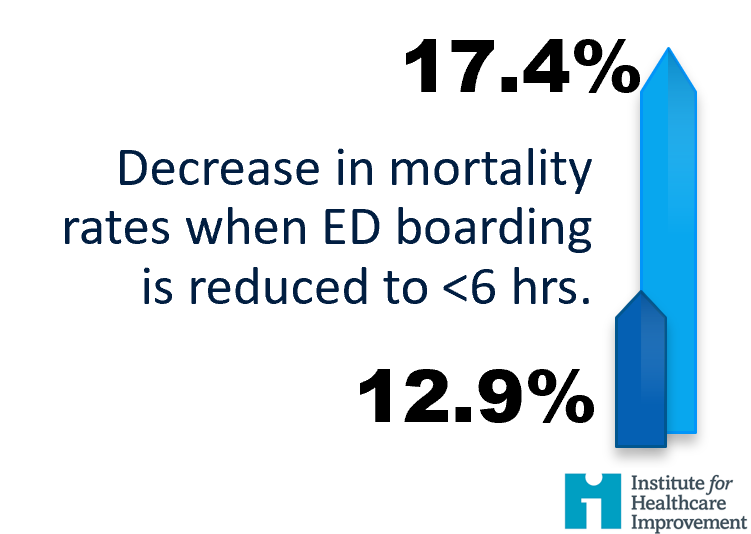
Timely onboarding is a major issue in hospitals around the world. According to the IHI, reducing ED boarding to under 6 hours reduced in-hospital mortality from 17.4% to 12.9% and reduced length of stay.[2]
Hospitals that provide an RTLS enabled patient tag can not only monitor patient wait times and alert to excessive waits (fig 1), they can also track the patient’s location and deliver messages related to their place in the queue. Capio St. Göran Hospital in Stockholm Sweden uses AiRISTA’s B4n messaging tag to manage patients waiting for surgery. The result was reduced delays, improved patient throughput, and increased patient satisfaction since patients gained the freedom to leave the waiting area.
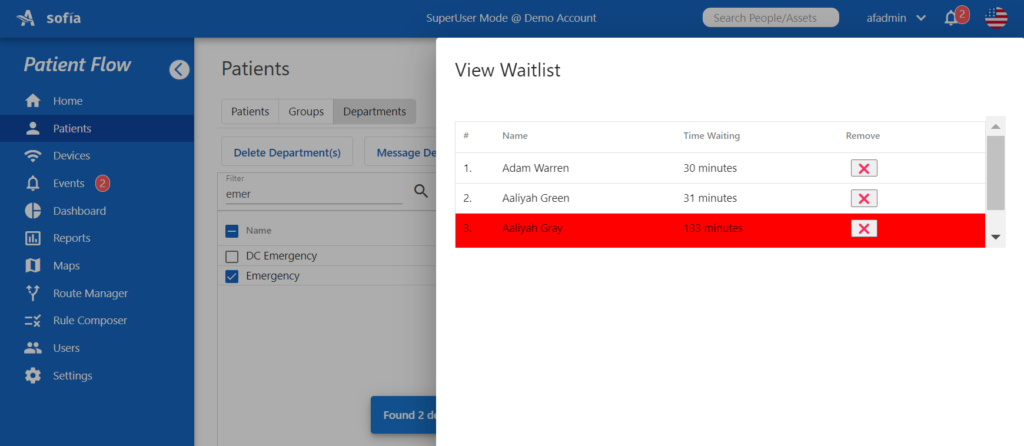
Fig.1 AiRISTA’s sofia RTLS platform alerts to wait times beyond a threshold
Improve the Efficiency of Patient Transport/Transfers

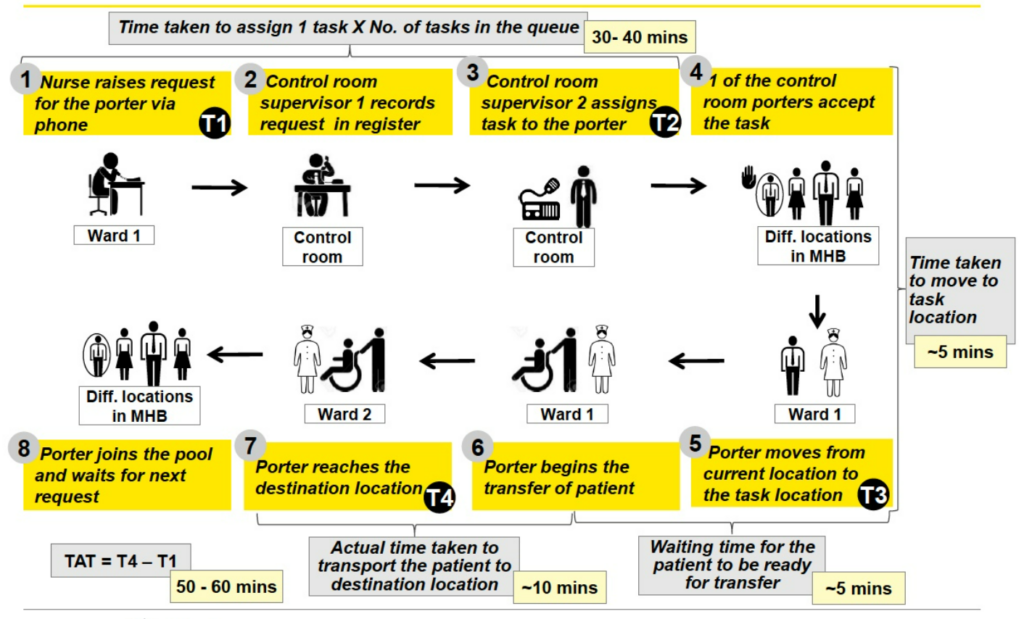
To relieve congestion in the waiting area and decrease boarding time, you can look to improvements in patient transport/transfers. AiRISTA partner, IceGen, deployed a workflow solution at India’s Manipal Hospitals. Using AiRISTA’s B4n personnel tags, nurses press a button to initiate a request.
The IceGen platform uses RTLS location information to dispatch the nearest available porter, basically an Uber like service. Once the request is complete, the porter pushes a button to close the request and timestamp the activity. Based on a study by Ernst & Young, turnaround times that were typically 50-60 minutes were reduced by 40% , the efficiency of the Patient assistants have increased up to 70% and the operational cost has reduced by 36%. According to Anand Surana, CEO of Icegen, “using a powerful device the B4n tag is the key. The solution is so affordable that many more staff members can participate in workflows than might not otherwise.”
Porter Efficiency Improvement
- Number of Requests 11,353/month
- Hours for completion 1,554 hours
- Hours Saved (50% improvement) 777 hours
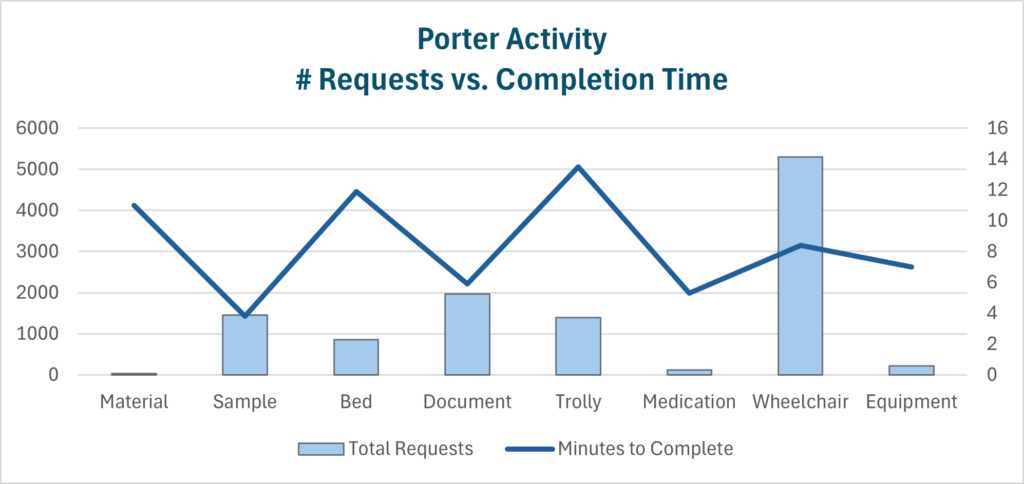
Nursing Efficiency Improvement
- Number of Calls per Day 500
- Minutes Saved per Call 10
- Minutes Saved per Month 130,000 (2,167 hours)
Improving Patient Discharge
Patient discharge is a complicated process that requires the coordination of patient, staff and equipment, and family. With all of these moving parts, it’s easy to understand the opportunities for inefficiency. With an RTLS solution like AiRISTA’s sofia platform, complex workflows like patient discharge are simplified by utilizing event triggers, staff and potentially family messaging, and location zone alerts to smoothly orchestrate activities to turn the patient room. Click here for a demonstration of the following:
- A porter alerted to the nearest wheelchair
- Event trigger to indicate the patient has physically left the room
- Dispatch environmental services to the room
- Return the room to the “available” state once cleaned
A well orchestrated patient discharge workflow can save over 4 hours of what would otherwise be a soiled room left idle. According to the IHI, a 275-bed hospital that manages to reduce the average stay by just four hours will accomplish the “equivalent to increasing physical capacity by ten beds.” If the average daily patient cost is $2,000, the hospital can increase its annual revenue by $7.3million.

Fig. 2 AiRISTA’s sofia RTLS platform’s Bed Management user module
Conclusion
AiRISTA isn’t alone in pushing the benefits of a better orchestrated patient flow. Gartner has developed the Real Time Health System Maturity Model to evaluate the HDO’s ability to “acquire and act on real-time operational intelligence to achieve its business objectives.” The model describes four levels along the maturity continuum. Levels 1 & 2 describe HDOs that are “reactive” or simply “monitor” changes to real time dynamics. According to Gartner, patient throughput and capacity management describe more advanced HDOs who have evolved to levels 3 & 4 in the maturity model where workflows are automated, and the organization becomes predictive. Using an RTLS solution like AiRISTA’s sofia platform helps providers migrate from tradition RTLS track and trace capabilities (levels 1 & 2) to being able to support workflows where patients, staff and equipment are organized around the end-to-end patient journey.
[1] Gartner, “Put Patient Throughput and Capacity Management at the Center of Your Performance Improvement Plan”, Barry Runyon, January 2021.
[2] Rutherford PA, Anderson A, Kotagal UR, Luther K, Provost LP, Ryckman FC, Taylor J. Achieving Hospital-wide Patient Flow (Second Edition). IHI White Paper. Boston, Massachusetts: Institute for Healthcare Improvement; 2020.





